SLEEP STUDY FAQ (ANSWERED BY A REGISTERED POLYSOMNOGRAPHIC TECHNOLOGIST)
By Amanda Jones RPSGT
If you have questions about undergoing a sleep study, you’re not alone. Here are some FAQ that I get asked while working at Comprehensive Sleep Care Center as a Sleep Technologist. They may be able to help you understand the process and put you more at ease.
A sleep study, known as a polysomnogram, is an overnight test done in a sleep lab. Prior to the study, a sleep technologist will place sensors on your scalp, face, chest and legs. These sensors will record brainwave activity (to assess sleep stage), eye movements, muscle activity, heart rhythm, body movements, nasal/oral airflow, respiratory effort and oxygenation. In addition, your body position will be observed on video camera. All this information will better assist your sleep physician in determining the cause of any sleep related problems.
Sleep Study FAQ
Q: WHY DO I NEED A SLEEP STUDY?
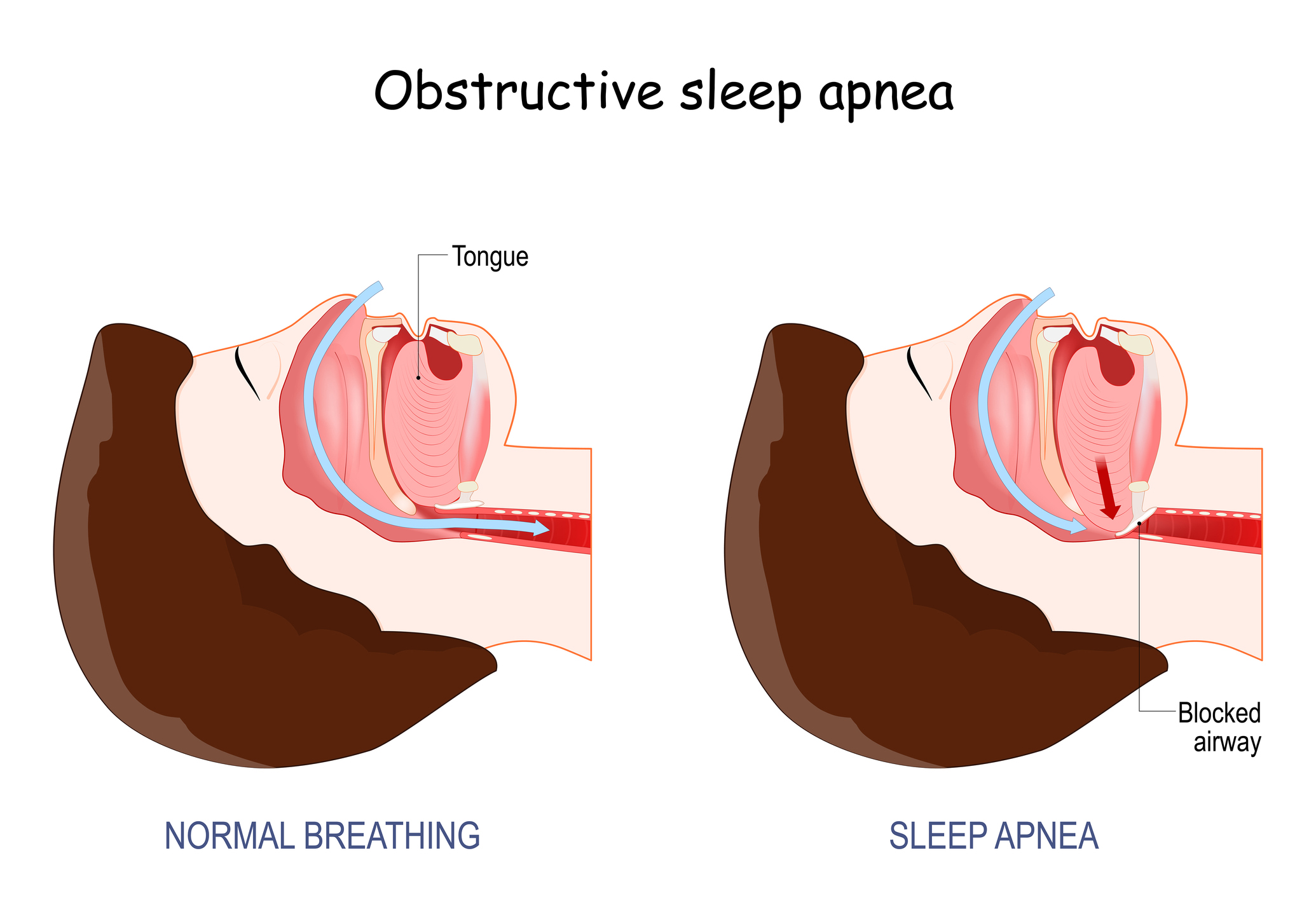
A: Sleep studies help doctors diagnose sleep disorders such as sleep apnea, periodic limb movement disorder, narcolepsy, restless legs syndrome, insomnia, and nighttime behaviors like sleepwalking and REM sleep behavior disorder.
Q: CAN MY SPOUSE OR SIGNIFICANT OTHER STAY WITH ME ON THE NIGHT OF MY STUDY?
A: Significant others may have helpful insight during the evaluation stage, but they are not usually permitted to stay with you on the night of your study. IF there is a reason they need to stay, please discuss it with your doctor during your consult.
Q: WHAT IF I CAN’T SLEEP?
A: Don’t stress, we don’t expect you to sleep as well as you would at home, and we take that into account. Nearly everyone can fall asleep during an in-lab study. In most cases, you do not need a full 6 hours of sleep for the doctor to make a diagnosis. There are several things you can do to help you sleep the night of your study. First consider waking a little earlier than usual on the day of your study. Do not take naps during the day. Avoid the consumption of all caffeine—skipping coffee, tea, soda pop, chocolate, energy drinks, and other caffeinated products.
Q: CAN I BRING MY OWN PILLOW?
A: Of course! We want you to be as comfortable as possible so you can sleep. Our sleep labs use My Pillows on each bed (one soft and one firm). However, most people prefer their own pillow. In fact, if you have a special blanket or throw you sleep with, bring that as well! The more comfortable you feel the better you will sleep.
Q: WHAT ABOUT ALL THE WIRES? WILL THEY STAY ON ALL NIGHT?
A: After you arrive at the sleep center a technician will apply small sensors to your head and body with adhesive. The wires connecting the sensors to a headbox are usually gathered to the side with plenty of slack so you can move around during sleep. Elastic belts will be wrapped around your chest and abdomen to measure breathing. A clip will be placed on your finger or (in some cases your earlobe) to monitor oxygen levels in your bloodstream. Most people get used to it all very quickly. Everything is attached using medical tape and/or paste. The wires are attached to stay on all night. If anything does come loose the tech will enter the room to re-attach them during the night. We attempt to do this without waking the patient if possible. The sensors are attached to your body in a manner like electrocardiogram (EKG) electrodes and are not painful. In rare instances, some people with sensitive skin develop local irritation at the electrode sites. If you have experienced skin irritation due to EKG testing in the past, or have an adhesive allergy please notify the Sleep Center and the technologist prior to the study.
Q: CAN I SLEEP ON MY SIDE? WHAT IF I MOVE AROUND IN MY SLEEP?
A: We want you to sleep in your natural position. Many people roll over and change positions multiple times during the night. While sleep apnea is more prevalent when sleeping on your back, the Technician may ask you to try sleeping on your back for a portion of the test. This allows us to check your breathing in multiple positions. IF you’re unable to, don’t worry! It may be very difficult to sleep on your stomach so the technician may ask you to use a pillow to keep you from rolling all the way onto your stomach.
Q: DURING MY SLEEP STUDY, WHAT IF I HAVE TO USE THE RESTROOM?
A: If you need to get up during your sleep study just notify your sleep technologist (by calling out or sitting up in the bed) and let them know that you need to use the restroom. They will unhook one or two central connections, which will enable you to get up and walk to the bathroom. The headbox even has a strap you can carry over your shoulder or around your neck. (The headbox is the device that all your wires connect into)
Q: MAY I SLEEP NAKED?
A: No. As a courtesy to our sleep techs we request that you sleep in pajamas or a t-shirt and shorts.
Q: HOW LONG IS THE SLEEP STUDY? WHAT IF I WAKE UP EARLY? CAN I SLEEP IN?
A: The wake-up time is 5 am, and unfortunately, we cannot allow patients to sleep in. Insurance requires a minimum of 6 hours of recording, and as long as we have reached that, you are free to leave before 5 am (some restrictions may apply depending on if the patient took a sleeping medication). Many people ask why they must get up so early. Our Sleep Technicians need to ensure all patients are up and checked out so they can upload all the data to be read and get home so they too can get some sleep.
Q: HOW HARD IS THE PASTE TO GET OUT OF MY HAIR?
A: The paste is water soluble! You can use a hairbrush, but some paste will remain. The best thing to do is wash your hair with very warm water. We recommend using conditioner first to loosen up the paste and then washing your hair. Rubbing alcohol is also an effective, quick way to remove paste but can be rough on the scalp. Also, Micellar water can be effective and less harsh.
Q: CAN THEY TELL ME THE RESULTS OF MY SLEEP STUDY IN THE MORNING?
A: Unfortunately, no. The sleep technologist is collecting data that will be interpreted by your sleep medicine physician. You will receive your results at your follow-up visit.
Whether you were a little nervous about your upcoming sleep study, or just curious about the process, we hope this cleared up a few questions and put your mind at ease! Remember, your Comprehensive Sleep Care Center sleep technologist is not only there to gather information, but they are there to make the process as comfortable as possible! We look forward to seeing you soon!